Walking is probably the simplest, most accessible way to manage blood sugar levels. For people with diabetes, a daily walk can really change how their body handles glucose.
Taking a 10-minute brisk walk after meals can help improve your post-meal blood sugar and reduce those annoying spikes right after eating.
Engaging in walking for blood sugar control not only aids in post-meal glucose management but also fosters a healthier lifestyle overall.

Popular posts:
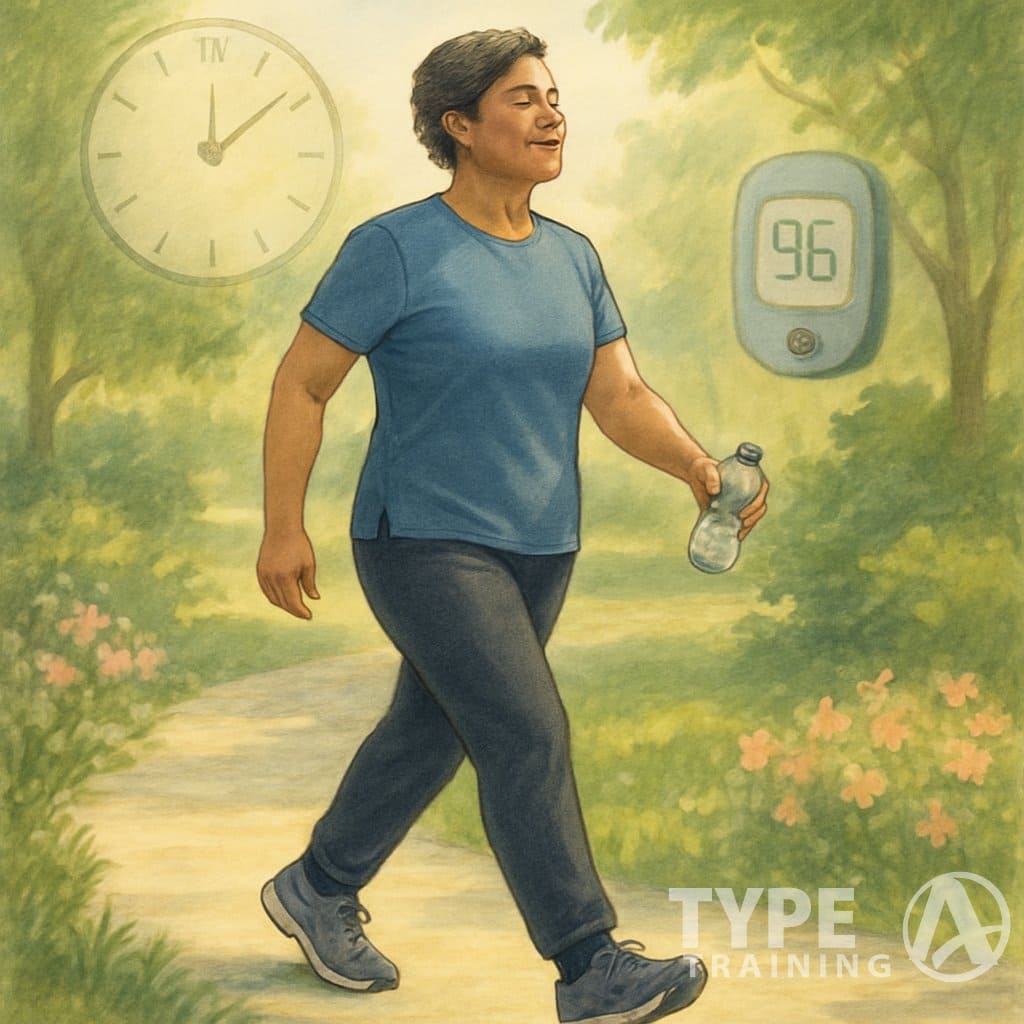
When you walk matters almost as much as the walking itself. Research suggests that three short walks after meals can be just as effective at reducing blood sugar over 24 hours as one longer walk.
Try to get at least 30 minutes of walking each day, and it’s totally fine to break that up into smaller sessions. Walking at a brisk pace (faster than 20 minutes per mile) has been linked to a 41% lower risk of type 2 diabetes.
Key Takeaways
- A 10-minute walk after meals can seriously reduce blood sugar spikes and help with overall glucose control.
- Aim for 30 minutes of daily walking, split into three 10-minute sessions after breakfast, lunch, and dinner.
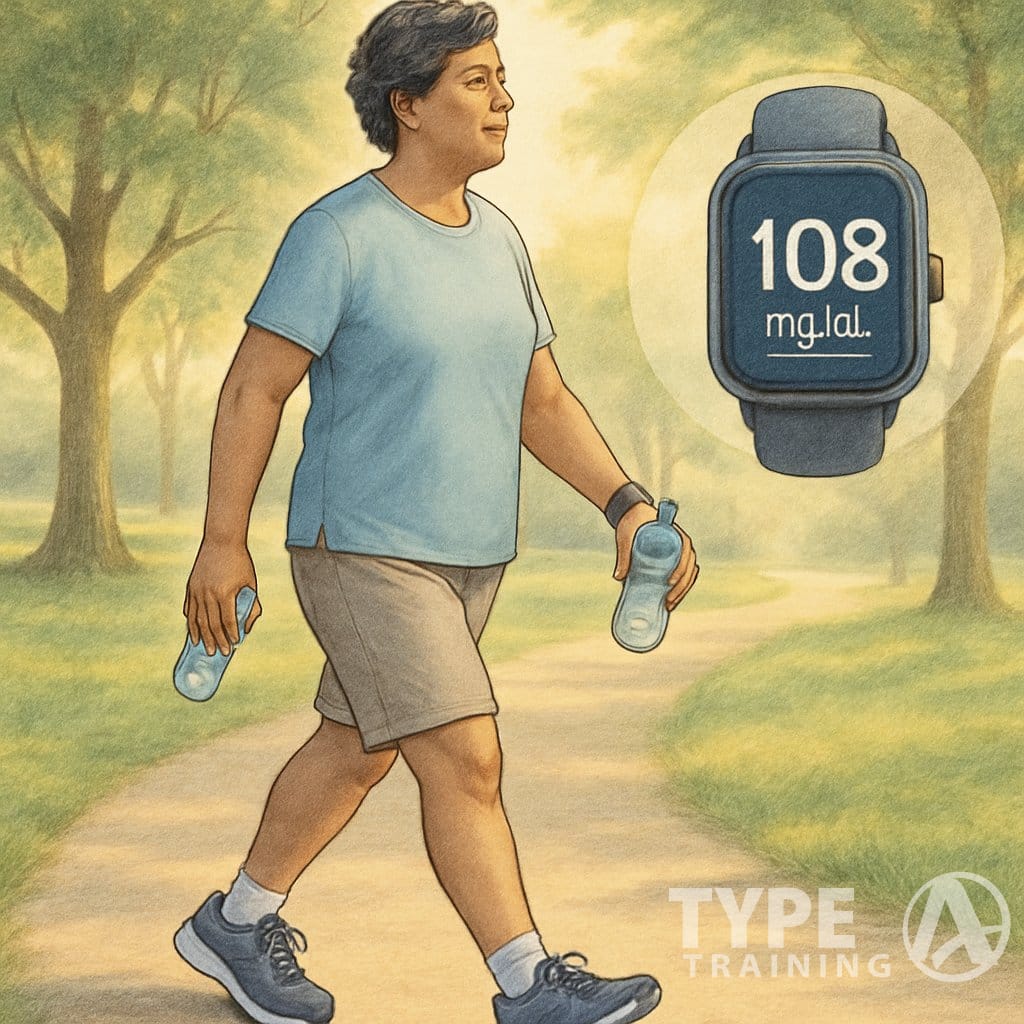
- Check your blood sugar before and after walking to see how your body responds, then tweak your routine as needed.
Why Walking Matters for Blood Sugar Control: Understanding the Importance of Walking for Blood Sugar Control

Walking stands out as one of the most effective ways to manage blood sugar. Regular walks, especially walking for blood sugar control, help your body process glucose more efficiently and support better health overall.
Walking for blood sugar control is a crucial practice for managing diabetes and improving overall health.
Walking for blood sugar control has proven to be an essential activity for managing diabetes effectively and enhancing quality of life.
Incorporating walking for blood sugar control into your routine can lead to better health outcomes and improved diabetes management.
Incorporating walking for blood sugar control into your routine can lead to better health outcomes.
Benefits of Walking for Diabetics
Walking gives people with diabetes plenty of advantages. You don’t need fancy equipment and you can do it pretty much anywhere.
When you make walking a habit, your body gets better at using insulin. Your cells pull more glucose out of your bloodstream.
Walking after meals works especially well. Even a short stroll after eating prevents extreme blood sugar spikes that can damage blood vessels in the long run.
Walking is gentle on your joints and rarely causes injury, making it a solid choice for all ages and fitness levels.
Impact on Glucose and Insulin Sensitivity
Walking directly affects how your body handles glucose. As you move, your muscles use glucose for energy, which lowers blood sugar.
Regular walks improve your insulin sensitivity, so your body doesn’t need as much insulin to deal with the same amount of glucose.
Walking activates special glucose transporters in your muscle cells. These help move glucose from your blood into your muscles.
Studies show that supervised walking programs lead to better glucose control for people with Type 2 diabetes. Even short walks—10 to 15 minutes—can help manage blood sugar.
Walking and Cardiometabolic Health
Walking strengthens your heart and boosts your overall cardiometabolic health. With regular walking, your heart pumps blood more efficiently.
This is key since people with diabetes face a higher risk of heart disease. Walking helps lower this risk by improving heart health.
Walking also helps with:
- Lowering
blood pressure - Reducing harmful cholesterol
- Decreasing inflammation in blood vessels
- Keeping your weight in check
All these benefits add up. Walking can provide substantial health benefits with much less risk than intense workouts.
Thirty minutes of walking, five times a week, can really move the needle on your cardiometabolic markers and help manage diabetes.
Optimal Timing for Walking to Lower Blood Sugar

When you walk can make a big difference in how well you lower your blood sugar. Strategic timing throughout the day helps keep glucose levels steady and improves insulin sensitivity, both short-term and long-term.
Walking After Meals
Walking after you eat is probably the best time to lower blood sugar. A post-meal walk helps muscles soak up glucose, which brings down both blood sugar and insulin.
Even a quick 10-minute walk can have a noticeable effect. Research finds that walking after meals can lower blood sugar by about 12% compared to taking one long walk at another time.
This effect stands out most after dinner or carb-heavy meals. If you can, start your walk within 30 minutes of finishing your meal—your body is busy digesting and dealing with glucose right then.
Just a 10-minute stroll after eating can help tame blood sugar spikes, and it’s easy to fit into a busy day.
Morning vs. Evening Walks
Morning walks help kickstart your metabolism and may set you up for better insulin sensitivity all day. Walking before breakfast seems to help with fasting blood sugar.
Evening walks, especially after dinner, offer the biggest benefits for blood glucose control. They help prevent those overnight blood sugar spikes that can sneak up on you.
Honestly, the best time is whenever you can stick with it. Consistency beats perfection.
Everyone’s body reacts a bit differently, so try checking your blood sugar before and after walks at different times to see what works for you.
Frequency of Daily Walking
Spreading your walks out during the day keeps blood sugar more stable than just one long session. Multiple short walks help you avoid big glucose swings.
Shoot for 15 to 30 minutes of total walking each day. This can lower blood sugar for up to 24 hours.
Breaking it into two or three shorter walks often works better than one long one. Your step count matters, too. Try for 7,500–10,000 steps per day if you can, but even adding 1,000 steps can help.
Consistency is key: daily walking gets you better results than occasional bursts of exercise. Make it part of your routine—maybe a quick walk after each meal.
If you’re just getting started, begin with short walks and slowly ramp up the time and pace as you get fitter.
Effective Walking Techniques for Diabetics
Walking the right way can help you manage blood sugar more effectively. Using good techniques and the right tools makes a real difference.
Moderate vs. Light-Intensity Walking
Intensity matters when you’re walking for diabetes. Moderate exercise works better than light walking.
A brisk pace—faster than 20 minutes per mile—links to a 41% lower risk of type 2 diabetes. But how do you know if your pace is right? You should be able to talk but not sing, and your breathing should be a bit heavier.
For best results, go for a pace that feels challenging but doable. Many experts suggest:
- Heart rate at 50–70% of your max
- Slightly sweaty after 10 minutes
- You can talk, but it takes effort
Light walking still helps, especially if you’re just starting out. Even slow walks after meals help with post-meal blood sugar.
Using a Pedometer or Treadmill
Tracking your walks can boost your motivation and results. A pedometer counts steps and keeps you honest about daily activity.
You can use:
- Free smartphone apps
- Fitness watches or bands
- Simple clip-on step counters
A pedometer shows your progress and helps you stay on track. Many devices also track distance, calories, and even sleep.
Treadmills are great when the weather’s bad. You can control your speed and track your heart rate. Many treadmills have built-in programs for different goals.
When you use a treadmill, start with a five-minute warm-up at a slow speed. Gradually ramp up to your target pace. Adding a slight incline (1-2%) makes it feel more like outdoor walking and is easier on your joints.
Achieving Your Step Goals
The 10,000 steps per day target is popular for a reason, but your goal should fit your own fitness level.
Start with what you can do. If you usually walk 3,000 steps, try for 4,000 before you think about 10,000. Small increases help prevent injury and burnout.
Some ideas to get more steps:
- Park farther away
- Take the stairs
- Walk during phone calls
- Set a reminder to move every hour
If a 30-minute walk feels like too much, break it up. Ten minutes in the morning, afternoon, and evening still adds up.
Track your progress week by week so you see the bigger picture. Celebrate the little wins as you build your walking habit.
Planning and Monitoring Your Walking Routine
A structured walking plan helps you get the most out of your efforts. Planning, tracking, and getting medical advice all play a role in staying safe and seeing results.
Creating a Personalized Walking Plan
Set realistic goals based on where you are now. If exercise is new for you, start with just 10 minutes of walking after meals—this helps your muscles use glucose and brings down blood sugar.
As you get fitter, slowly add more time and pick up the pace. The American Diabetes Association says it’s fine to split your walks if 30 minutes all at once feels tough—try 10 minutes in the morning, afternoon, and evening.
Think about these elements for your plan:
- Frequency: Try to walk every day
- Timing: Post-meal walks (15–30 minutes after eating) work great
- Duration: Build up to 30 minutes total per day
- Intensity: Aim for a pace where you can talk but not sing
Tracking Blood Sugar Responses
Check your blood glucose before and after walking to see how exercise changes your levels. Keep a simple log with the details:
Blood Sugar Walking Log
| Time | Before Walk | After Walk | Notes |
|---|---|---|---|
| Date | Reading | Reading | How you felt |
Notice how different walking times affect your numbers. Morning walks might impact blood sugar differently than evening walks.
Try a fitness tracker or a phone app to keep tabs on steps, distance, and heart rate. Studies say higher step counts make it easier to reach your blood glucose goals.
Involving Your Health Care Team
Talk to your healthcare provider before starting a new exercise routine. They’ll help spot any risks based on your health and medications.
Bring your walking logs and blood sugar readings to appointments. Your doctor can help you make sense of the results and suggest changes to your walking plan or meds if needed.
Ask about walking recommendations that fit your situation. Sports medicine specialists may suggest different strategies depending on your:
- Fitness level
- Diabetes complications (if any)
- Other health issues
- Medication schedule
Check in with your health care team regularly so your walking program keeps supporting your diabetes management as things change.
Safety Considerations and Complications
When you walk with diabetes, you need to watch for certain risks. A little preparation and knowing what to expect can make your walks safer and more enjoyable.
Managing Hypoglycemia and Blisters
Hypoglycemia (low blood sugar) can pop up during or after walking. Check your blood sugar before, sometimes during, and after exercise—especially if you take insulin or other meds that lower blood glucose.
Watch for these hypoglycemia signs:
- Shakiness or trembling
- Sweating
- Hunger
- Confusion
- Weakness
Always carry fast-acting carbs like glucose tablets or juice. If your blood sugar dips below 70 mg/dL, use the 15-15 rule: eat 15 grams of carbs, wait 15 minutes, then check again.
Blisters can be a nuisance. Check your feet every day and wear
Break in new
Walking with Diabetic Neuropathy
Diabetic neuropathy means you need to be extra careful. Nerve damage can dull feeling in your feet, so you might not notice injuries.
Key precautions:
- Check your feet before and after walks
- Wear supportive
shoes - Try cushioned insoles if you need them
- Start with short walks and build up slowly
If you have neuropathy, never walk barefoot—not even indoors. Pick
Take breaks on long walks to check your feet. If you spot redness, stop and let your feet rest. Moderate walking is usually safe once your foot ulcers have healed, but always double-check with your doctor.
Understanding Other Risks
Foot issues aren’t the only thing to watch for. Physical activity can affect your blood glucose for up to 24 hours by making your body more sensitive to insulin.
If you have prediabetes, regular walking helps lower your risk of progressing to type 2 diabetes. Still, keep an eye out for low blood sugar on longer walks.
People with diabetes sometimes face heart problems. Start slow, and pay attention to any chest pain, unusual shortness of breath, or dizziness.
Drink water before, during, and after your walk. Dehydration can mess with blood sugar and make things riskier.
Breaking up long sitting periods with quick walks throughout the day can lower blood sugar and cut down on complications. It’s a good strategy if you can’t fit in long walks.
Long-Term Health Benefits and Lifestyle Motivation
Walking regularly can change your health in ways that go way beyond blood sugar. It boosts your energy, mental wellbeing, and even protects you from big stuff like heart disease.
Maintaining Stamina and Energy Levels
Walking often builds stamina over time, so you feel more energetic during the day. As you stick with it, your body gets better at using oxygen, which helps your endurance.
Your muscles get stronger, and your heart and lungs adapt to deliver oxygen more efficiently. That means you won’t tire out as quickly doing everyday stuff.
Walking after meals can really help your energy since it keeps blood sugar spikes (and crashes) in check. Start with 10-minute walks and add more time as you get used to it.
Morning walks can set the tone for a good day, while evening strolls might help you wind down and sleep better.
Mental Health and Balance
Walking does wonders for your mental health. When you walk, your brain releases endorphins—those natural chemicals that boost your mood and lower stress.
People with diabetes who walk daily often report less depression and better mental health. The steady rhythm of walking can feel meditative and clear your head.
Getting outside adds another layer of benefit. Sunlight helps regulate mood and sleep, and green spaces seem to melt away mental fatigue.
Try walking in nature if you can. Walking with friends or family adds a social element, which is great for your mood and sense of balance.
Preventing Heart Disease and Weight Gain
Walking tackles two big concerns for people with diabetes: heart disease and weight. Just 30 minutes a day can lower your
For weight control, walking burns calories but is gentle on your joints. Pairing a regular walking routine with healthy eating helps you maintain or lose weight.
Heart health is especially important for diabetics, who face higher risks. Walking strengthens your heart and boosts circulation.
If you want the most heart benefit:
- Aim for 150 minutes of walking each week
- Add some brisk walking to get your heart rate up
- Stay consistent—regular walks beat occasional intense efforts
Walking is one of the most approachable lifestyle changes for diabetes. It helps with blood sugar and long-term heart health.
Guidelines and Resources for Diabetic Walkers
Walking works well for blood sugar management if you have diabetes. Following the right guidelines and teaming up with health experts can help you get the most out of it and avoid problems.
Recommendations from the American Diabetes Association
The American Diabetes Association recommends regular walking. It helps your body use insulin and lowers your risk of complications.
They suggest aiming for at least 150 minutes of walking each week, spread across several days. That could mean five 30-minute walks or shorter 10-minute walks after meals.
Research points out that walking after meals is especially effective. Just 10 minutes after eating can lower blood sugar better than one long walk, especially if you ate a lot of carbs.
If you’re new to exercise, start slow. Begin with 5-10 minute walks and add more time or intensity as your fitness improves.
Collaborating with Your Health Care Team
Before you jump into a walking program, talk to your healthcare provider. They’ll check your fitness level and look for any diabetes-related complications that could mess with your plans.
Your doctor or diabetes educator can:
- Suggest the right walking intensity for your current health
- Tell you when and how to check your blood sugar before and after walks
- Help you figure out the best timing for your meds around your walks
- Offer tips for handling possible low blood sugar during exercise
A sports medicine specialist might chime in about footwear or walking techniques. That’s extra helpful if you deal with neuropathy or have any foot issues.
Keep checking in with your healthcare team. As you get fitter or your blood sugar changes, they can tweak your walking plan. Tracking your progress and bringing it to appointments can really help.