Lyme Disease and Long COVID have significant impacts on your health, particularly on your immune system.
If you’re struggling with symptoms from either of these illnesses, strengthening your immune system is crucial for recovery.
Managing Lyme Disease and Long COVID can be daunting, but you’re not alone.
Popular posts:
By introducing specific strategies and tools, you can support your body’s natural defenses and promote healing.
Whether through diet, supplements, or lifestyle changes, taking proactive steps can make a substantial difference in how you feel daily.
The journey to recovery might seem long, but it’s achievable with the right approach.
You need practical, actionable tools that fit into your lifestyle and enhance your well-being.
In this post, we’ll explore seven essential tools that can aid in boosting your immune system and helping you navigate the challenges associated with Lyme Disease and Long COVID.
Understanding Lyme Disease and Long COVID
These two conditions, while different, both stem from infectious diseases and can result in ongoing health challenges.
Knowing the basics about Lyme Disease and Long COVID will help you navigate their impacts and improve your health management strategies.
Lyme Disease: An Overview
Lyme Disease originates from the bacterium Borrelia Burgdorferi, transmitted through tick bites.
Ticks, mainly black-legged ticks, contract the bacteria from infected animals and pass it to humans.
Initial symptoms may include fever, headache, fatigue, and a skin rash called erythema migrans.
If left untreated, infection can spread to joints, the heart, and the nervous system.
Early diagnosis and antibiotic therapy are crucial for effective treatment. Regular tick checks and protective clothing can prevent Lyme Disease.
Long COVID: Definition and Symptoms
Long COVID refers to prolonged symptoms following infection with the virus SARS-CoV-2.
These symptoms persist for weeks or months after the acute phase of the illness and can affect anyone, regardless of initial infection severity.
Common symptoms include fatigue, shortness of breath, brain fog, and joint pain.
The exact causes of Long COVID are still under investigation, but they likely involve ongoing inflammation or immune response.
Comparing the Conditions
Both Lyme Disease and Long COVID involve infectious agents—bacterial in Lyme and viral in COVID-19.
While Lyme transmission involves tick bites, Long COVID stems from initial infection with SARS-CoV-2.
Symptoms may vary, but fatigue and joint pain are common in both.
Treatment approaches differ, with Lyme focusing on antibiotics and Long COVID requiring multifaceted management.
Importantly, while Lyme has a clear microbial cause, Long COVID mechanisms are more complex and not fully understood.
Immune System Challenges
Both Lyme Disease and Long COVID can significantly impact your immune system.
Understanding how these diseases interact with your immune response is key to managing symptoms and finding effective treatments.
The Role of the Immune System in Lyme Disease and Long COVID
Your immune system plays a crucial role in combating infections.
In Lyme Disease, the bacterium Borrelia burgdorferi triggers an immune response that can sometimes become chronic.
Long COVID, on the other hand, involves prolonged immune activation even after the virus is no longer present.
The immune response in both conditions can vary widely. Chronic Lyme can lead to persistent symptoms due to an ongoing immune battle. Similarly, long COVID’s lingering effects can be linked to a continuous, overactive immune response.
Inflammation and Autoimmunity
Inflammation is your body’s natural reaction to infection or injury.
In Lyme Disease, inflammation caused by the bacterium can lead to symptoms like joint pain and fatigue.
Long COVID patients often experience similar inflammatory responses.
Autoimmunity occurs when your immune system mistakenly attacks your own tissues.
Both Lyme Disease and Long COVID can trigger autoimmune reactions, complicating the healing process. Symptoms may include neurological issues or chronic pain.
Addressing inflammation and autoimmune responses is crucial.
Anti-inflammatory treatments and immune-modulating therapies can offer relief and improve quality of life.
Biomarkers and Immune Response
Biomarkers can help track your immune response to infections.
In Lyme Disease, specific antibodies against Borrelia burgdorferi can be indicative of an ongoing immune battle.
Long COVID research is identifying biomarkers like cytokines that signal chronic inflammation.
Following biomarkers allows for a targeted treatment approach.
Blood tests can reveal levels of inflammation, autoantibodies, and other immune factors.
This information helps you and your healthcare provider make informed decisions about your treatment plan.
Monitoring your biomarkers provides insight into how your immune system is functioning.
This ongoing assessment is vital for managing chronic conditions and optimizing your recovery.
Symptomatic Similarities and Differences
Lyme disease and Long COVID share various symptoms, making diagnosis challenging. Both conditions may affect neurological, cognitive, and physical functions.
Common Symptoms
Both Lyme disease and Long COVID can present with fatigue, brain fog, and muscle aches.
Patients often report extreme tiredness that doesn’t improve with rest. Brain fog can manifest as difficulty concentrating, poor memory, and confusion. Muscle aches are common in both conditions, causing discomfort and impacting daily activities.
Despite these similarities, there are distinctions. Lyme disease might include a distinct erythema migrans rash, which Long COVID does not. The presence of this rash could be a crucial indicator differentiating Lyme from other illnesses.
Neuropsychiatric Symptoms and Cognitive Impairment
Neuropsychiatric symptoms such as anxiety, depression, and mood swings occur in both conditions but can vary in severity.
Cognitive impairment, or brain fog, is frequent in both, characterized by impaired judgment, lengthened reaction times, and confusion.
Lyme disease may lead to severe neurological issues like facial palsy, whereas Long COVID often involves persistent cognitive difficulties without such specific neurological signs.
This differentiation is vital for healthcare providers when diagnosing these conditions based on neurocognitive symptoms.
Physical Impairments and Chronic Pain
Lyme disease and Long COVID can lead to significant physical impairments.
Chronic pain, particularly joint pain, is a hallmark of Lyme disease, often described as arthritic.
Patients with Long COVID might experience chronic pain but not necessarily as joint-specific.
Mobility can be impacted in both conditions. Lyme disease may cause swelling and inflammation in joints, leading to prolonged discomfort.
Long COVID often leads to generalized weakness and muscle pain that hampers physical activity.
Understanding these distinctions aids in tailoring patient care effectively.
Diagnostic Approaches
Accurate diagnosis of Lyme Disease and Long COVID requires specific tests and understanding of symptoms.
Learn about the different methods used to identify these conditions and their challenges.
Detecting Lyme Disease
Lyme Disease is typically diagnosed through clinical evaluation and laboratory testing.
Enzyme-linked immunosorbent assay (ELISA) is often the first step, detecting antibodies against Borrelia burgdorferi.
If positive, it is followed by the Western Blot test to confirm the diagnosis.
Polymerase Chain Reaction (PCR) is another method used to detect bacterial DNA in body fluids.
Biomarkers like certain proteins in the blood can also indicate Lyme Disease.
Early detection is crucial to prevent chronic issues like arthritis and neurological complications.
Identifying Long-Haul COVID
Long COVID, also known as Post-Acute Sequelae of SARS-CoV-2 infection (PASC), presents varied symptoms.
Diagnosing this condition relies on a combination of persistent symptoms and ruling out other causes.
Persistent symptoms may include fatigue, brain fog, joint pain, and others, lasting for weeks or months post-infection.
Laboratory tests do not yet have specific biomarkers for Long COVID.
Research is ongoing to identify consistent patterns and biomarkers that could aid in diagnosing this condition more reliably.
Current diagnosis primarily involves detailed history taking and the exclusion of other potential conditions.
Challenges in Diagnosis
Diagnosing Lyme Disease and Long COVID presents significant challenges.
Both conditions can exhibit symptoms similar to other diseases, complicating identification.
Dendritic cells and other immune markers are being studied to improve diagnostic precision.
False positives and negatives are common, especially in the early stages of infection.
Standard tests may miss early Lyme Disease due to the delay in antibody production. For Long COVID, the lack of a clear definition and standard biomarkers adds to the complexity.
Accurate and early diagnosis is essential for effective management and treatment.
Studies are ongoing to improve diagnostic approaches and identify novel biomarkers to aid in the more precise detection of these conditions.
Treatment Strategies
Effective strategies for managing Lyme Disease and Long COVID include targeted approaches to address specific symptoms and innovative treatments to enhance immune system function.
Managing Lyme Disease
Treatment for Lyme Disease primarily involves antibiotics.
Early detection and use of doxycycline, amoxicillin, or cefuroxime axetil can prevent complications.
For persistent symptoms, known as Post-Treatment Lyme Disease Syndrome (PTLDS), extended antibiotic courses may be needed.
Post-treatment care is crucial.
Physical therapy aids muscle and joint recovery. Stress management techniques, such as mindfulness and yoga, improve overall well-being.
For children, paying attention to Pediatric Acute-onset Neuropsychiatric Syndrome (PANS)—sometimes linked to Lyme Disease—is essential, requiring specialized care.
Combatting Long COVID
Long COVID often leads to symptoms like fatigue, cough, and palpitations.
Treatment focuses on symptom management and boosting immune function.
Respiratory therapies, including breathing exercises, help with lingering coughs.
For heart issues, particularly palpitations, beta blockers or calcium channel blockers can be effective under a doctor’s supervision.
Rehabilitation programs, involving both physical and cognitive activities, support return to everyday life.
Supplements like Vitamin D and Zinc may enhance immune resilience, as some studies suggest.
Innovation in Treatment Approaches
New treatments and research continue to emerge.
Gene therapy and immunotherapy show promise in both Lyme Disease and Long COVID. These approaches aim to boost the body’s natural defense mechanisms.
Monoclonal antibodies are an area of interest, potentially neutralizing lingering infections.
Adaptogens and herbal treatments, like astragalus and echinacea, may support the immune response.
Continual monitoring of treatment efficacy and adapting to new research findings is vital.
Engaging with healthcare professionals who specialize in Lyme Disease and Long COVID ensures that you receive the most current and effective care strategies.
Lifestyle and Home Remedies
Supporting your immune system involves targeted strategies.
Focus on nutrition, personalized exercise programs, and mindfulness practices.
Nutrition and Diet
Eating a balanced diet can significantly impact your immune system.
Consuming foods rich in antioxidants, such as berries, nuts, and leafy greens, may help reduce inflammation.
Incorporate omega-3 fatty acids from sources like salmon and flaxseed to support cognitive function and reduce the risk of depression.
Avoid processed foods and sugars that can negatively affect your immune response.
Instead, choose whole foods and consider probiotics like yogurt or fermented vegetables to promote gut health, essential for overall immune function.
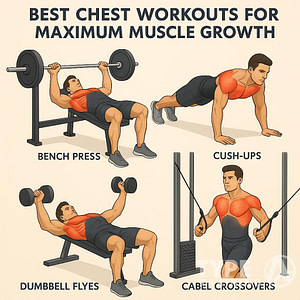
Exercise and Physical Rehabilitation
Regular physical activity can improve your immune system and mental health.
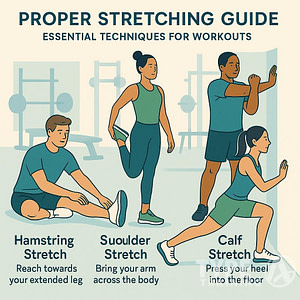
Low-impact exercises like walking, swimming, or yoga help increase circulation and reduce inflammation.
Create a routine that fits your lifestyle and start slowly, especially if you are recovering from illness.
Strength training under the guidance of a professional can aid in rebuilding muscle.
Physical activity also alleviates symptoms like insomnia, anxiety, and depression, enhancing your overall quality of life.
Mental Health and Mindfulness
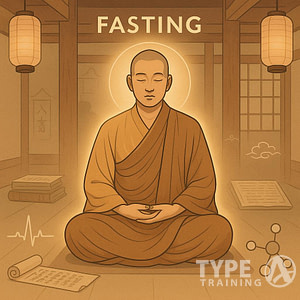
Mindfulness practices such as meditation, deep breathing, and progressive muscle relaxation can reduce stress and anxiety.
High stress levels negatively affect immune function and might exacerbate symptoms like headaches and insomnia.
Develop a daily routine that includes these practices.
Consider guided meditation apps or mindfulness workshops to help establish consistency.
Engaging in hobbies and social activities also promotes well-being, contributing to a stronger immune response.
Therapeutic Developments and Research
Recent strides in medical research have shed light on the various therapies and interventions available to manage symptoms and improve the quality of life for individuals with either Lyme disease or Long COVID.
Current Research in Lyme Disease
Recent studies have focused on better understanding the complex nature of chronic Lyme disease.
Researchers are exploring biomarkers that can help in early diagnosis and effective treatment strategies.
Innovative treatments, such as immunotherapy and antibiotic combinations, are being tested to combat persistent symptoms.
Additionally, research is investigating the role of co-infections that complicate Lyme disease management.
Data collection from large, diverse populations is crucial in these studies.
This makes the findings more applicable and improves treatment options.
Next-generation sequencing and other advanced technologies are playing a critical role in these developments.
Breaking Ground on Long COVID Research
Long COVID research is in its early stages, but significant progress has been made in identifying predictors and long-term effects.
Scientists are exploring the persistence of symptoms like fatigue and cognitive impairments.
Key studies focus on how SARS-CoV-2 affects different body systems, aiming to develop targeted therapies.
Recent findings suggest immune dysregulation may be a core factor, guiding novel therapeutic approaches such as anti-inflammatory medications and antiviral treatments.
Clinical trials are ongoing to evaluate the effectiveness of these interventions.
Collaboration across global research institutions is accelerating our understanding and treatment of Long COVID.
Funding and Future Directions
Funding plays a pivotal role in advancing research for both Lyme disease and Long COVID.
Governments, private organizations, and philanthropic entities have significantly increased investment in these areas.
Future research directions include large-scale studies and international collaborations to foster a comprehensive approach.
Emphasis is on developing predictive models and therapeutic interventions that are precise and personalized.
Emerging technologies, such as artificial intelligence and machine learning, will likely drive future discoveries.
The integration of these technologies aims to streamline data analysis and improve treatment outcomes.
Researchers continue to seek sustainable funding sources to support long-term studies, which are essential for identifying effective treatments and ultimately improving patient care.
Prevention and Public Health
Preventing Lyme Disease and COVID-19 involves specific actions to protect yourself and others. This encompasses safeguarding against tick bites, adhering to COVID-19 protocols, and enhancing awareness through education.
Protecting Against Ticks
To prevent Lyme Disease, the first step is avoiding tick bites.
When outside in wooded or grassy areas, wear long sleeves and pants with tight cuffs.
Use insect repellent containing DEET or permethrin on clothing and exposed skin.
After returning indoors, perform a thorough tick check on yourself, children, and pets.
Pay close attention to areas like the scalp, behind the ears, and armpits.
Shower soon after being outdoors to wash away ticks before they attach. If you discover a tick, remove it promptly with fine-tipped tweezers.
COVID-19 Precautions
To reduce the risk of COVID-19 infection, follow public health guidance.
Vaccination remains one of the most effective measures. Ensure you receive all recommended doses for optimal protection.
Wear a mask in crowded or enclosed spaces, and maintain a safe distance from others where possible.
Regularly wash your hands with soap and water for at least 20 seconds, or use hand sanitizer with at least 60% alcohol.
Stay informed on local COVID-19 trends and adhere to any specific guidelines or recommendations issued by health authorities.
Awareness and Education
Increasing awareness about Lyme Disease and COVID-19 is crucial for prevention.
Utilize resources from reliable sources such as Lymedisease.org and follow their Facebook Page for updates and community support.
Stay informed through credible public health websites and attend webinars or community events on disease prevention.
Promote educational campaigns in your community to highlight the importance of protective measures and early detection.
Schools, workplaces, and local organizations can play a pivotal role in spreading knowledge.
Encourage others to engage in preventive practices and seek accurate information.
Maintaining community awareness ensures everyone is better equipped to protect themselves and reduce the spread of these illnesses.
Impact of Chronic Conditions on Daily Living
Chronic Lyme Disease and Long COVID can affect daily life in many ways. Persistent symptoms such as headaches and shortness of breath may interfere with social, professional, and personal activities.
Navigating Social and Professional Hurdles
Living with chronic conditions often means dealing with unpredictable symptoms.
Headaches and fatigue can make it challenging to focus at work. Shortness of breath may limit your ability to participate in social gatherings or professional events.
Coworkers and friends might not fully understand your limitations, leading to feelings of isolation.
You may need to communicate your needs clearly and seek adjustments at work, such as flexible hours or remote work options.
Improving Quality of Life
Managing chronic conditions involves both medical and lifestyle adjustments.
Regular exercise, while sometimes difficult, can improve your energy levels.
Balanced nutrition can support your immune system, helping your body to combat inflammation and regulate cytokines.
Mindfulness and relaxation techniques may reduce stress and improve your resilience.
Maintaining a routine that includes enough rest is essential.
Small, consistent changes can add up to significant improvements in how you feel daily.
Patient Support and Resources
Accessing proper support and resources is crucial.
In the United States, patient advocacy groups can connect you with others experiencing similar challenges.
Support groups provide a platform to share experiences and solutions.
Healthcare providers specializing in Chronic Lyme Disease and Long COVID can offer tailored treatments.
It’s also valuable to stay informed through reliable sources, ensuring that you have the latest information on managing your condition effectively.
Genetics and Personalized Medicine
Advances in genetics and personalized medicine aim to tailor treatments to individual immune responses. This can improve outcomes for conditions with varying presentations like Lyme Disease and Long COVID.
Genetic Factors in Immune Response
Genetics play a significant role in how your immune system responds to infections.
Specific genes can act as predictors for susceptibility to Lyme Disease and Long COVID.
For instance, variations in HLA genes can influence chronic symptoms.
Familial studies have shown that some genetic combinations may provide better resistance or a more robust immune response to these illnesses.
In the United States, researchers focus on identifying these genetic markers to aid in early diagnosis.
Biomarkers derived from genetic information can improve the precision of treatment strategies.
Personalized Treatment Considerations
Personalized medicine involves tailoring treatment plans based on genetic factors.
Genetic testing can help identify which medications will be most effective for you.
For Lyme Disease and Long COVID, some therapies may be beneficial only for individuals with certain genetic markers.
This approach minimizes trial-and-error in treatment, reducing the risk of side effects.
Pharmacogenomics, the study of how genes affect your response to drugs, is crucial.
This science helps clinicians prescribe medications that align with your genetic makeup, potentially improving recovery rates.
Emerging Technologies in Diagnostics
Emerging technologies are revolutionizing diagnostics in personalized medicine.
Tools like next-generation sequencing offer detailed genetic profiles, paving the way for more accurate diagnostics.
Machine learning algorithms analyze genetic data to identify biomarkers associated with chronic symptoms.
These biomarkers help in predicting disease progression and tailoring treatments.
In the United States, these technologies are increasingly integrated into clinical practice, offering more precise diagnostic options.
Investing in these tools may improve patient outcomes by enabling more targeted and effective interventions.
Exploring Co-Infections and Secondary Conditions
Understanding co-infections and secondary conditions is crucial for managing Lyme Disease and Long COVID. Factors like latent viruses and additional infections can complicate the immune system’s recovery process.
The Role of Latent Viruses
Latent viruses, such as the Epstein-Barr Virus (EBV), can reactivate under stress or immune suppression. This reactivation can cause symptoms akin to primary infections.
Managing these latent viruses is essential, as they can deplete your immune resources and prolong recovery.
EBV is linked to both Lyme Disease and Long COVID. Being aware of its impact can help tailor treatments effectively.
Other latent viruses can also play a significant role in inhibiting your recovery, making them an important aspect of patient care.
Co-Infections in Lyme Disease and Long COVID
Co-infections like Borrelia Burgdorferi, the causative agent of Lyme Disease, can exist alongside other infectious diseases. These co-infections can exacerbate fatigue, pain, and cognitive issues.
In Long COVID, bacterial and viral co-infections can severely impact symptoms.
The interaction between co-infections and primary infections complicates diagnostics and treatment plans.
Identifying and managing all present infections ensures a more comprehensive and effective approach to recovery.
Impact on the Immune System
Co-infections and secondary conditions heavily affect your immune system. They can lead to immune dysregulation, making you more susceptible to further infections.
Both Lyme Disease and Long COVID involve a complex interplay of immune responses.
Chronic infections can weaken immune defenses, requiring vigilant monitoring and management to prevent worsening conditions.
Understanding how these factors impact your immune system can guide better, more personalized treatment strategies.
Regulatory and Advisory Perspectives
Understanding the regulatory and advisory perspectives on Lyme Disease and Long COVID can help you navigate healthcare directives more effectively. These guidelines shape how you might approach treatment and disease management.
Centers for Disease Control and Prevention (CDC) Guidelines
The CDC provides comprehensive guidelines on managing both Lyme Disease and Long COVID.
For Lyme Disease, the CDC recommends early diagnosis and antibiotic treatment. Their guidelines detail preferred antibiotics, dosages, and treatment duration.
For Long COVID, the CDC emphasizes monitoring symptoms and working closely with healthcare providers.
They also suggest staying up-to-date with vaccinations and continuing hand hygiene practices. Regular check-ups help manage ongoing symptoms and prevent complications.
Global Health Organizations’ Views
Global health organizations like the World Health Organization (WHO) and the European Centre for Disease Prevention and Control (ECDC) also offer valuable guidelines.
The WHO focuses on global surveillance and prompt treatment of Lyme Disease, underscoring the importance of tick-bite prevention.
For Long COVID, both WHO and ECDC stress the need for ongoing research and individualized care plans.
They advocate for international collaboration in sharing data and best practices to improve patient outcomes.
Patient Advocacy and Disease Reporting
Patient advocacy groups play crucial roles in raising awareness and pushing for improved treatments. Organizations like the Global Lyme Alliance campaign for faster, more accurate diagnostics and better patient support.
Disease reporting is also vital. Accurate data submissions to health departments help track the prevalence of Lyme Disease and Long COVID.
This collective data aids in refining treatment protocols and improving public health responses.
Lyme Disease & Long COVID: How Personal Training Can Help
Personal training can be instrumental in helping you manage Lyme disease and Long COVID symptoms. When your body feels fatigued or in pain, finding the right exercise routine can provide physical relief and emotional uplift.
A personal trainer tailors workout routines to your specific needs. They ensure that exercises are safe and effective for your condition, focusing on low-impact activities to minimize strain on your joints.
Staying motivated can be a challenge. A personal trainer offers the encouragement and accountability needed to keep you on track.
Their expertise helps you navigate the delicate balance between pushing your limits and avoiding overexertion.
Diverse Exercises
Engaging in a variety of exercises like yoga, pilates, and breath work can be beneficial.
These activities help increase flexibility, reduce tension, and improve overall well-being.
Type A Training in NYC offers instructors skilled in these areas to support your recovery journey.
Monitoring Progress
Personal trainers help you measure progress, making necessary adjustments along the way. Tracking improvements can boost your confidence and motivate you to continue.
Mind-Body Connection
Exercises such as meditation and breath work enhance the mind-body connection.
This is especially useful for managing symptoms of Lyme disease and Long COVID, promoting mental clarity and relaxation.
Relief from Symptoms
Regular exercise guided by a personal trainer can lessen symptoms like joint pain, fatigue, and stiffness. Incorporating routines such as swimming or stationary cycling are effective yet gentle on your body.
Frequently Asked Questions
This section will address common questions related to the relationship between Lyme disease and COVID-19, symptom differences, testing, and effective immune-boosting strategies.
Can COVID-19 exacerbate the symptoms of Lyme disease?
Yes, there is evidence suggesting that COVID-19 can worsen Lyme disease symptoms. Both conditions involve immune responses that could synergize, leading to heightened inflammation and other symptoms.
What are the symptoms associated with post Lyme disease syndrome?
Symptoms often include fatigue, joint and muscle pain, and cognitive difficulties. These can persist long after initial treatment, significantly impacting daily life.
How does chronic Lyme disease differ from the acute condition?
Chronic Lyme disease refers to symptoms that persist for months or years after the initial infection. Acute Lyme disease is the early stage and is usually more responsive to antibiotics.
What are the most reliable tests for diagnosing Lyme disease?
The two-tiered serology test, which includes the ELISA test followed by a Western blot, is considered the gold standard for diagnosis. PCR tests can also be useful in certain cases.
What are considered the severe symptoms of Lyme disease?
Severe symptoms can include neurological problems such as meningitis, facial palsy, and arthritis in large joints. In rare instances, Lyme carditis, which affects the heart, can occur.
Which immune-boosting strategies are effective for Lyme disease patients?
Maintaining a balanced diet, regular exercise, and adequate sleep are key strategies.
Supplements like vitamin D and C, along with probiotics, can also support your immune system.
Consulting healthcare providers about personalized plans is advisable.